Abstract
Background. The use of a space maintainer during the deciduous dentition period at a proper time can prevent the consequences of the loss of the arch length in the future. There is controversy over the use of space maintainers.
Objectives. The aim of this study was to evaluate the magnitude of stresses exerted on immature permanent molar teeth, and the extent of displacement of these teeth when the adjacent teeth are missing, but after placing a space maintainer. Studies carried out to date have used clinical measurements, e.g., X-rays and dental casts.
Material and methods. The finite element model (FEM) was used for modeling the maxillary and mandibular teeth and the bone structure. A space maintainer (band and loop) was also designed for modeling. Force was applied and a finite element analysis (FEA) was carried out in 6 states in the maxilla and in the mandible to evaluate the distribution of stresses and the amount of displacement of immature permanent first molar teeth in the presence or absence of deciduous second molar teeth and a space maintainer.
Results. During mastication, when the deciduous second molar tooth was absent, the maximum stress was transferred to incomplete roots. When there was a space maintainer, stress was transferred to the space maintainer itself and to the distal side of the deciduous first molar tooth. The displacement of permanent first molar teeth was minimal in the presence of all teeth; in the absence of the deciduous second molar tooth, this displacement increased 4–5-fold, which decreased again almost to the level of the 1st/4th state (intact arch) in the presence of the space maintainer.
Conclusions. The results showed the importance of the use of space maintainers, as they significantly decrease the momentary displacement of the teeth as well as the stress exerted on the developing permanent first molar teeth.
Key words: finite element analysis, space maintenance, mesial tooth movement
Introduction
Space management is a crucial issue in pediatric dentistry.1 Local or systemic factors can lead to the early loss of deciduous teeth, including tooth extractions due to caries, traumatic injuries, and premature exfoliation resulting from abnormal root resorption and systemic disorders. Space reduction after the premature loss of primary second molars is one of the important factors affecting the occurrence of malocclusion, often increasing a demand for orthodontic treatment.2 The premature loss of deciduous second molars has the most significant effect on the dental arch, and the maximum space loss is due to the mesial drift of permanent first molar teeth.3 The use of a space maintainer during the deciduous dentition period at a proper time can prevent the consequences of the loss of the arch length in the future.4 It has been reported that the space change after the premature loss of a primary second molar in 3 weeks is statistically significant.5 A primary second molar is an eruption guide for a permanent first molar, so with the early loss of this guidance, a severe space loss will occur. The fastest and the greatest space closure occurs in the maxilla, followed by the mandible.6
There is controversy over the use of space maintainers. Some researchers believe that space maintainers are not useful and have detrimental effects in 19% of cases.7 There are a number of ill effects of conventional band and loop space maintainers – they lead to plaque retention, which causes gingivitis, the blanching of the gingivae due to band displacement, mucosal overgrowth, and loop impingement on the mucosa, causing pain and ulceration.8 Bilateral space maintainers may have questionable efficacy, and in case of the loss of multiple molars in the same quadrant, their use should be weighed against the risk of unwanted tooth movements, the loss of a removable space maintainer or no space maintenance at all.4
Space maintainers are mostly prescribed at a young age; their use is associated with some problems as a result of the patients’ poor compliance, the possible manipulation of these appliances, and even the risk of swallowing a separated segment of the wires used as well as with economic problems. Therefore, in some cases, parents are not interested in the use of such appliances.9
The masticatory force is defined as a force that is created through the dynamic action of the masticatory muscles during the act of chewing.10 The force of mastication depends on many factors, including age, gender, tooth developmental stage, and hardness of food. This force is maximum in the molar area. The alveolar bone is immature and more elastic in children, less calcified, and has fewer trabeculae and larger bone marrow spaces as compared to adults. In addition, the lamina dura is thinner and the interdental crest is flatter than in the case of adults.11 In the mixed dentition period, permanent first molar teeth in the maxilla and the mandible are still developing and erupting; the roots of these teeth are not completely mature, making them very different from mature teeth. When a tooth is subjected to the physiologic force of mastication, stresses are transferred to the underlying bone through the periodontal ligament (PDL). Mature teeth with their long roots provide a large area to transfer these stresses and they are distributed on all root surfaces. However, in teeth that are still developing, only a small surface area of the root is available for transferring similar forces to the underlying bone. Therefore, it is expected that higher stresses will be induced in PDL.12 The analysis of the biomechanical properties of the tooth can help us understand the pattern of functioning of the periodontal tissue during mastication, and in general, the masticatory function. Therefore, it is necessary to construct a model to unify the structural geometry of the teeth, the tissue characteristics and the forces applied to the jaws. It is now well established that a model accurately simulating all the above variables is able to provide very accurate results.13 Currently, the need for a model such as the finite element model (FEM) has attracted attention. So far, no study has evaluated the magnitude of stresses exerted on immature permanent molar teeth with short roots and open apices, and the extent of displacement of these teeth when the adjacent teeth are missing; in addition, this displacement has not been evaluated after placing a space maintainer. Studies carried out to date have used clinical measurements, and none of them have made accurate evaluations with the use of a finite element analysis (FEA). Furthermore, studies using FEA have been very limited, especially in children during the mixed dentition period on immature molars. The stresses considered normal for mature teeth might be different for an immature, developing tooth; in addition, there are differences between maxillary and mandibular first molars in terms of the extent of displacement and bodily movement of the teeth.
The aim of this study was to evaluate the magnitude of stresses exerted on immature permanent molar teeth, and the extent of displacement of these teeth when the adjacent teeth are missing after a space maintainer was placed. Studies carried out to date have used clinical measurements, such as X-rays and plaster models (dental casts).
Material and methods
A finite element analysis was designed and applied in the present study to evaluate stresses and the displacement of maxillary and mandibular first molars in the mixed dentition period under normal masticatory forces in the presence or absence of deciduous second molar teeth and a space maintainer. To this end and to carry out the study on both jaws, three-dimensional (3D) models of the teeth, the jaws and a band and loop space maintainer were constructed as follows.
Preparation of a 3D model of the teeth
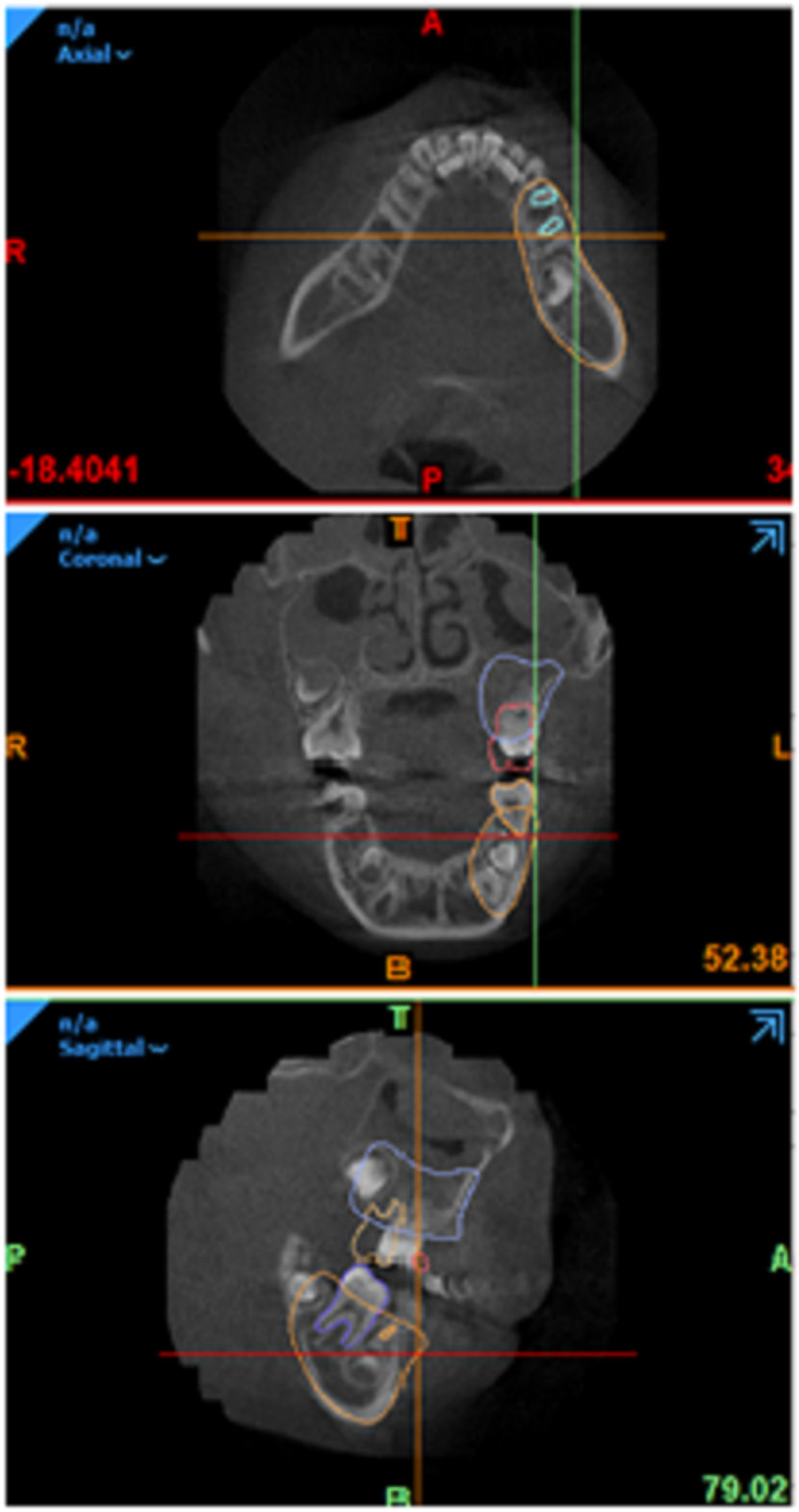
A 3D model was designed using the cone-beam computed tomography (CBCT) images of a 6-year-old child whose permanent first molar teeth had erupted recently and established in the occlusal relationship (Figure 1).
The model was designed accurately in its geometric dimensions, and deciduous first and second molars as well as permanent first molars were included in the model. The CBCT images were entered into a computer for processing 3D images, which converts CBCT and magnetic resonance imaging (MRI) data to 3D computer-aided design (CAD) models, and then the teeth were constructed. All tooth surface curves were recorded during the designing process, which resulted in an improvement in the accuracy of calculations in this model.
Preparation of a 3D model
of the periodontal ligament
After constructing a 3D model of the teeth, a 3D model of PDL was constructed with a thickness of 0.25 mm,14, 15 along the anatomic roots (Figure 2). The periodontal ligament was considered as a uniform mass with linear behavior. Although such a structure does not conform with the real biologic behavior of PDL, various studies have shown that this assumption, i.e., a uniform linear structure, is very valuable for assessing orthodontic forces and appears to be sufficient to explain the initial tooth movements.
Preparation of the bone surrounding
the tooth
The geometry of the maxilla and the mandible was constructed using the CBCT images of a 6-year-old child, and materials were assigned to the spongy- and compact-bone compartments. To design and construct the bone, it was considered as a solid and rigid body. Then, the tooth root–PDL complex was eliminated from this volume by using a complex process with the ‘subtract’ command (Figure 3).
Incorporation of the model for drawing
Geometric software was used to divide the teeth, which were in the form of surfaces, into solid segments. The 3D model was extracted in the SAT format, which could be read in the Essence milieu. With the FE package, point cloud data was converted into 3D volumes, and then all components were converted into the STP format for FEA.
Preparation of a model of a space maintainer
A band and loop space maintainer was used to this end. The geometry of the space maintainer was designed in the form of a 0.180 × 0.005-inch stainless steel band and a 0.36-inch stainless steel loop (Figure 4).
To prepare a geometric model for applying boundary conditions, and for meshing and loading, it is necessary to enter the characteristics of the materials forming each component into a computer. Table 1 presents the physical properties of the materials used in the present study.16
The contact between the components was considered complete and tie-bonded. The coefficient of friction between the tooth and the space maintainer was assumed to be 0.2.16
Automatic meshing
All the components of the 3D model were divided into smaller components (Figure 5). In addition, the areas subject to the concentration of tensions, such as the apical and alveolar crest areas, were constructed of smaller components to improve the accuracy of these points. The elements were constructed in the form of a tetrahedron. Table 2 presents the approximate number of knots in each component.
Application of force
Seventy-newton vertical forces (almost equal to the normal masticatory force) were applied to the mesiopalatal cusp of the maxillary permanent first molar and to the distobuccal cusp of the mandibular permanent first molar (Figure 6).
The different states of the model components were as follows:
- 1 – the maximum equivalent stress induced and the amount of displacement of the maxillary first molar in an intact arch in the presence of the deciduous second molar;
- 2 – the maximum equivalent stress induced and the amount of displacement of the maxillary first molar in the absence of the deciduous second molar;
- 3 – the maximum equivalent stress induced and the amount of displacement of the maxillary first molar in the presence of the space maintainer;
- 4 – the maximum equivalent stress induced and the amount of displacement of the mandibular first molar in an intact arch in the presence of the deciduous second molar;
- 5 – the maximum equivalent stress induced and the amount of displacement of the mandibular first molar in the absence of the deciduous second molar;
- 6 – the maximum equivalent stress induced and the amount of displacement of the mandibular first molar in the presence of the space maintainer.
Results
A static FEA was carried out in 6 states in the maxilla and the mandible to evaluate the distribution of stresses and the amount of displacement of immature permanent first molar teeth in the presence or absence of deciduous second molar teeth and a space maintainer.
The maximum equivalent stress and displacement of the permanent maxillary first molar are presented in Table 3.
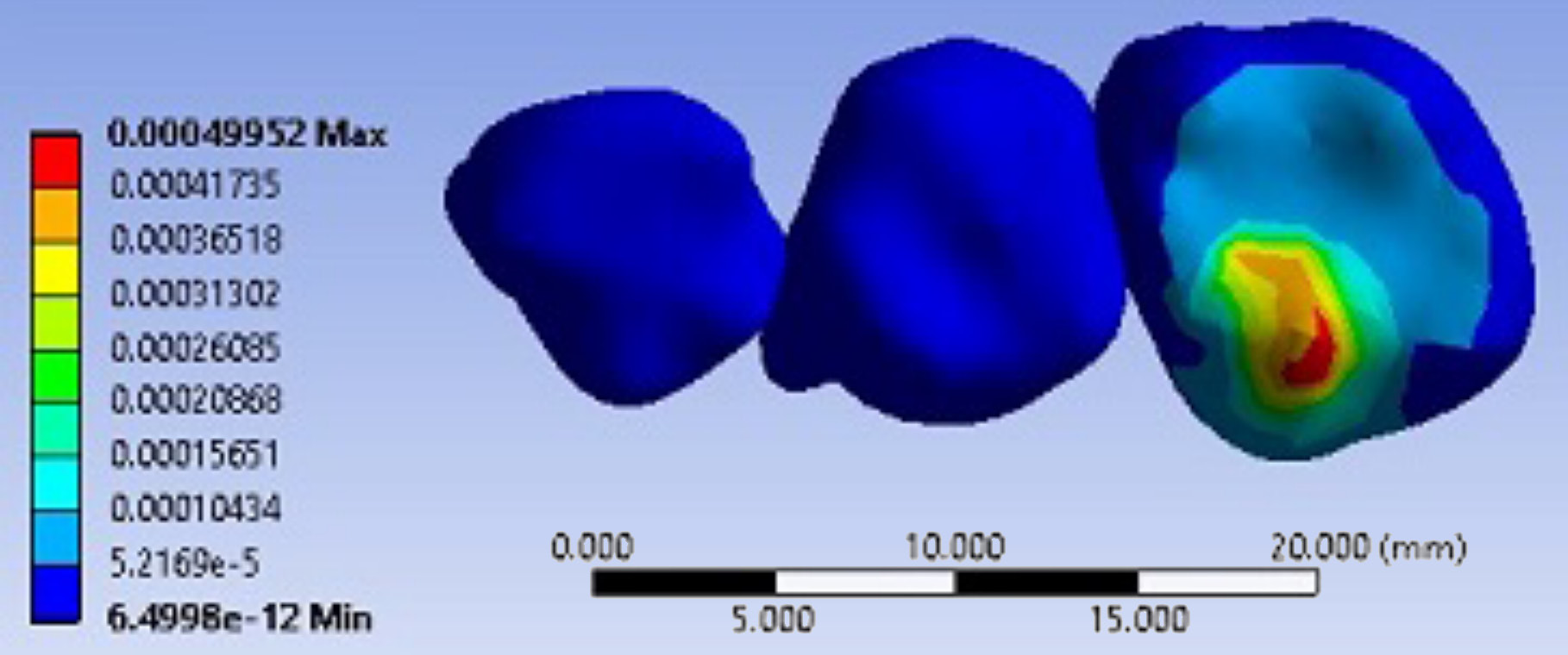
When a 70-N force was applied to the mesiopalatal cusp of the maxillary permanent first molar tooth in the presence of the deciduous second molar tooth, the maximum equivalent stress was recorded at the mesial contact of the crown at 50 MPa, and the other parts of the crown and PDL did not exhibit a considerable stress (Figure 7). The amount of displacement of the permanent first molar was only 0.5 µm (Figure 8).
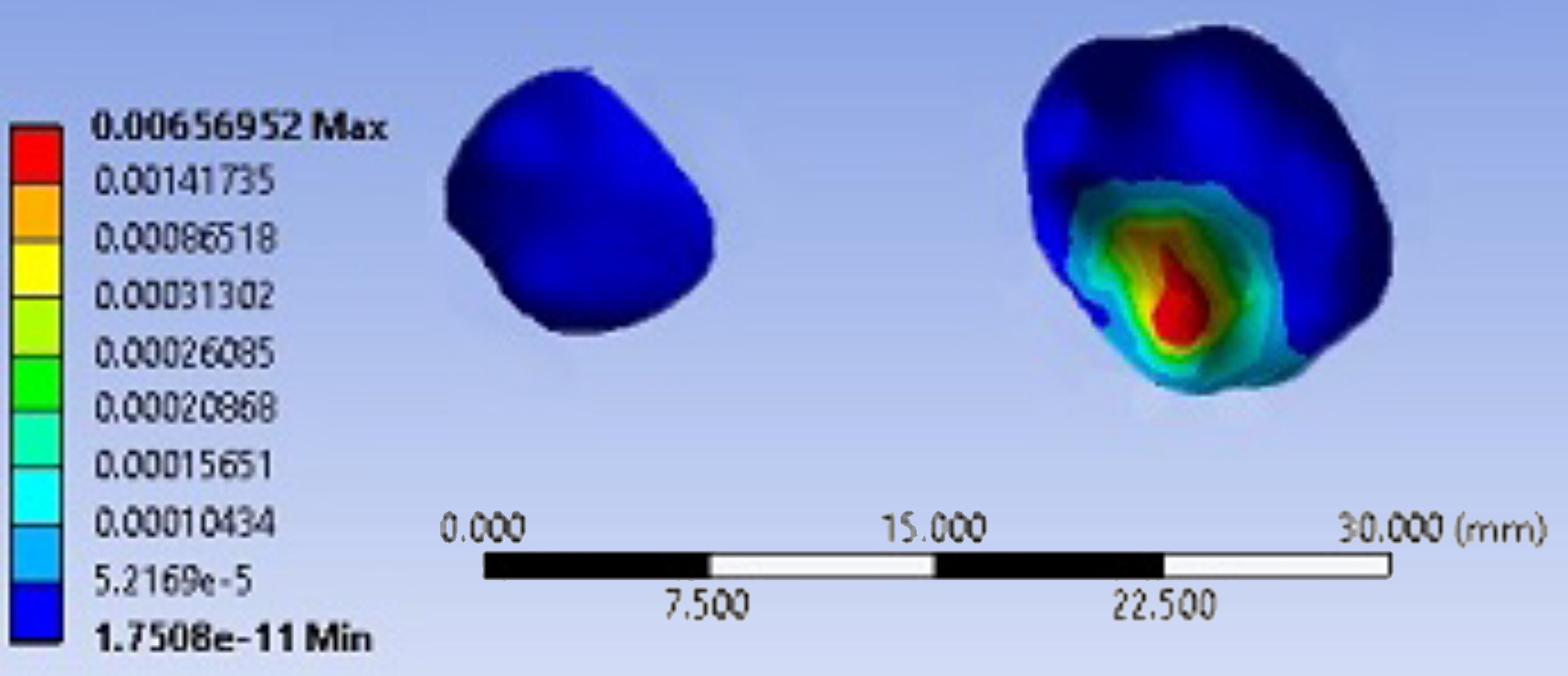
In the 2nd state, a 70-N force was applied in the absence of the deciduous second molar tooth. In this state, the maximum equivalent stress was recorded in the palatal root of the permanent first molar tooth at 12–16 MPa. The crown and the 2 other roots had a low level of stress (Figure 9). The displacement of the permanent first molar tooth increased in this state and was 6.5 µm in the mesiopalatal direction (Figure 10).
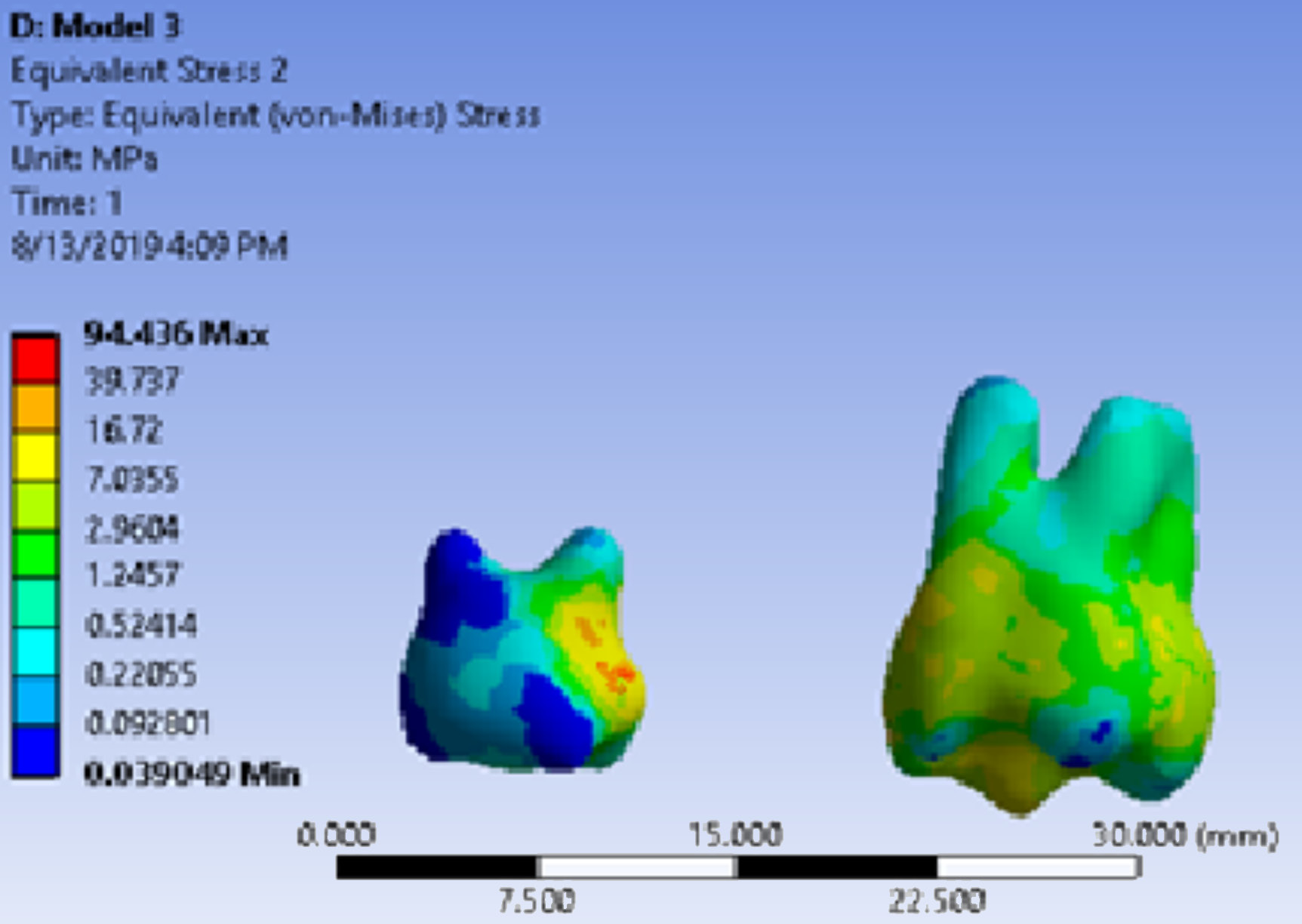
In the 3rd state, the force was applied in the presence of the space maintainer. In this state, the maximum equivalent stress on the permanent first molar tooth was recorded on the whole surface of the crown at 10–15 MPa, while the stress in PDL decreased. The maximum equivalent stress in this state was recorded on the surface of the space maintainer and on the distal aspect of the crown of the deciduous first molar tooth (94 MPa) (Figure 11). A displacement of 0.6 µm was recorded in this state (Figure 12).
The maximum equivalent stress and displacement of the permanent mandibular first molar are presented in Table 4.
When a 70-N force was applied to the distobuccal cusp of the mandibular permanent first molar tooth in the 4th state, i.e., in the presence of the deciduous second molar tooth, the maximum equivalent stress was recorded at the mesial contact of the crown at 75.5 MPa. The stress in the roots was similar at 5–6 MPa (Figure 13). Displacement in this state was 0.8 µm (Figure 14).
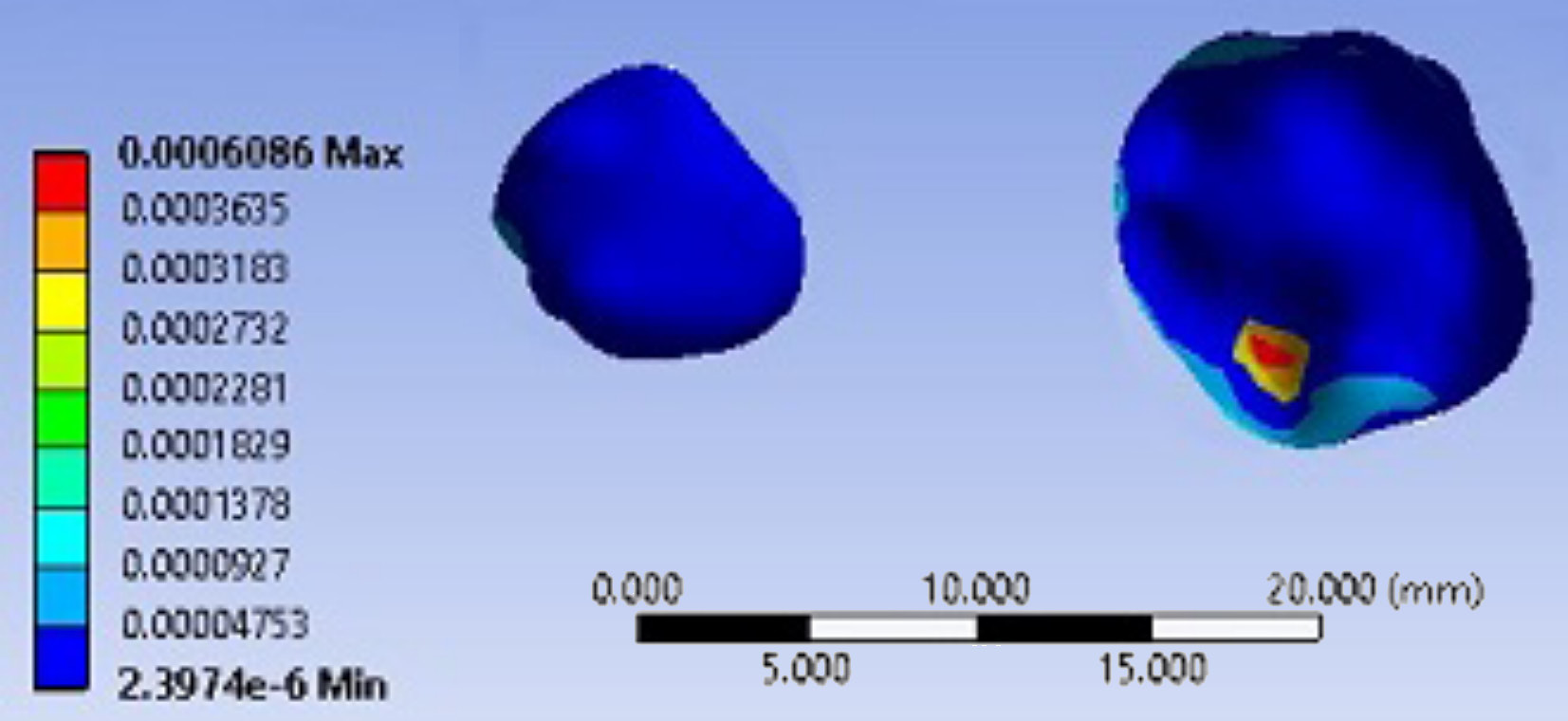
The force was applied in the 5th state, i.e., in the absence of the deciduous second molar tooth. In this state, the maximum equivalent stress at the cervical area of the mesial root was 14 MPa (Figure 15). Displacement in this state was 7.8 µm in the mesial direction (Figure 16).
In the 6th state, in which the force was applied in the presence of the space maintainer, the maximum equivalent stress on the entire crown surface was 10–12 MPa, while the root stress decreased to 5–6 MPa. In the mandible, too, a high rate of stress was applied to the space maintainer and the distal area of the crown of the deciduous first molar tooth (98 MPa) (Figure 17). Displacement in this state was 0.7 µm (Equation 18).
Discussion
In FEA, maxillary and mandibular permanent first molars were used to construct a model and simulate changes in the equivalent stress distribution pattern and displacement in the presence and absence of deciduous second molar teeth and a space maintainer.
This analysis is independent of time and shows changes on the spot. However, it is possible to determine changes in the shape of the models in terms of a time factor with the use of some frameworks. This analysis has some obvious advantages, including the fact that it can provide data consistent with real and clinical conditions, and confirm or refute it. Furthermore, it can measure some variables that cannot be observed and measured in real and clinical conditions.17
The normal masticatory force is significantly lower than the maximum bite force. The maximum bite force is defined as the maximum force that an individual can apply with their teeth, and is different from the normal masticatory force. In a normal child, this masticatory force is approx. 78 N.18 In the present study, this force for a 6-year-old child was considered at 70 N.
In an intact dental arch with all the teeth present in both jaws, the maximum equivalent stress was detected at the mesial contact of the permanent first molar tooth, which was transferred to the tooth mesial to the first molar, rather than to its roots. The tooth root, PDL and all the other areas of the tooth crown exhibited much lower stresses, which is consistent with the results of a study by Southard et al., who reported that the anterior component of the occlusal force (ACF) was transferred to the mesial teeth by a proximal contact and could even pass the midline.19 Chauhan et al. also reported similar results.12
The application of force resulted in the minor displacement of the roots of permanent first molars, and the tooth crown also exhibited a displacement of 0.5–1 µm, which is not clinically important and can be considered the physiologic displacement of the tooth during mastication. This finding is consistent with the results of clinical studies which showed that in the presence of all teeth, no significant displacement could take place.20
In the 2nd/5th state, in which deciduous second molars were not present in the dental arch, the maximum equivalent stresses in both arches were transferred to the roots, with higher stresses in the palatal root of the maxillary tooth, followed by the mesiobuccal root. In the mandible, the mesial aspect of the mesial root exhibited the maximum equivalent stress, followed by the mesial aspect of the distal root. These stresses were maximum in the cervical area and the apical area of the roots, which is consistent with the results of a study by Dejak et al., who reported that the maximum stresses during mastication were produced in the occlusal area and in the cervical area of the lingual aspect of permanent first molars in the mandible.21 In addition, Petcu et al. carried out a study on subjects during the mixed dentition period and reported that the maximum stress was detected in the cementoenamel junction (CEJ) area and in the coronal third of the root.17 Such a discrepancy between the results of studies might be attributed to differences in the anatomy of the teeth and the different developmental stages of immature permanent first molar teeth.
In this state, the maximum equivalent stresses were recorded in the mandibular permanent first molar as compared to the maxilla.
When a permanent first molar tooth is not in contact with a deciduous second molar tooth, the momentary tooth displacement increases 4–5-fold, which is mostly visible in the crown area, while the roots are displaced at a lower rate. Therefore, both maxillary and mandibular permanent first molars tend to tip mesially, rather than move bodily, which was confirmed in the present study and reported in previous clinical studies.22 In studies by Chauhan et al.12 and Kojima and Fukui,23 the FEA of maxillary permanent first molar teeth showed that the mesial tipping of these teeth was greater than their bodily movement. In the present study, such displacement of maxillary first molars was observed in the mesiopalatal direction, with only mesial displacement in the case of mandibular first molars.
The comparison of displacement between the 2 jaws showed that the displacement of the lower first molar was greater than that of the upper first molar, which does not coincide with the results of previous clinical studies.1, 5 It can be concluded that, although momentary displacement in the mandible is greater than in the maxilla, more displacement will occur in the maxilla over time due to the more spongy nature of the maxillary bone.
The amount of displacement of the roots was much smaller than that of the tooth crown, and the displacement of the roots of the mandibular first molar was lesser than in the case of the maxillary first molar, indicating much fewer bodily movements in the mandible as compared to the maxilla. Chauhan et al. also recorded some bodily movement in maxillary first molar teeth.12
When the force was applied in the presence of the space maintainer, stresses on the crown and the roots decreased significantly, and were transferred to the space maintainer itself. In addition, high stresses were recorded in the distal aspect of the crowns of deciduous first molars. In the present study, stresses in the distal aspect of the deciduous mandibular first molar were higher than those in the distal aspect of the corresponding tooth in the maxilla. Such a difference might be explained by differences in the anatomy of the teeth between the 2 jaws.
The amount of tooth displacement that was recorded in this state decreased almost to that from the 1st/4th state in an intact arch, and tooth tipping, which was observed in the absence of second primary molars and without mesial constraint, decreased significantly. However, a small amount of root displacement is not clinically important.24
The results of the present study showed that when a permanent first molar tooth erupts, if a deciduous second molar tooth is not in contact with the mesial aspect of the erupting tooth, a large amount of the arch length will be lost and the space will be closed over time. No study to date has evaluated the equivalent stresses exerted on the tooth, the space maintainer and the distal aspect of the deciduous second molar tooth. The results of the present study showed the pattern of distribution of the equivalent stress during mastication; the results also showed that space maintainers are useful in preventing the momentary displacement of the teeth.
Conclusions
The results showed the importance of the use of space maintainers, as they significantly decrease the momentary displacement of the teeth as well as the stress exerted on the developing permanent first molar teeth.